The challenges facing spine surgery
Spine surgery still defined by misplaced screws, radiation, lost OR time, and high costs — risks no tool has yet solved.
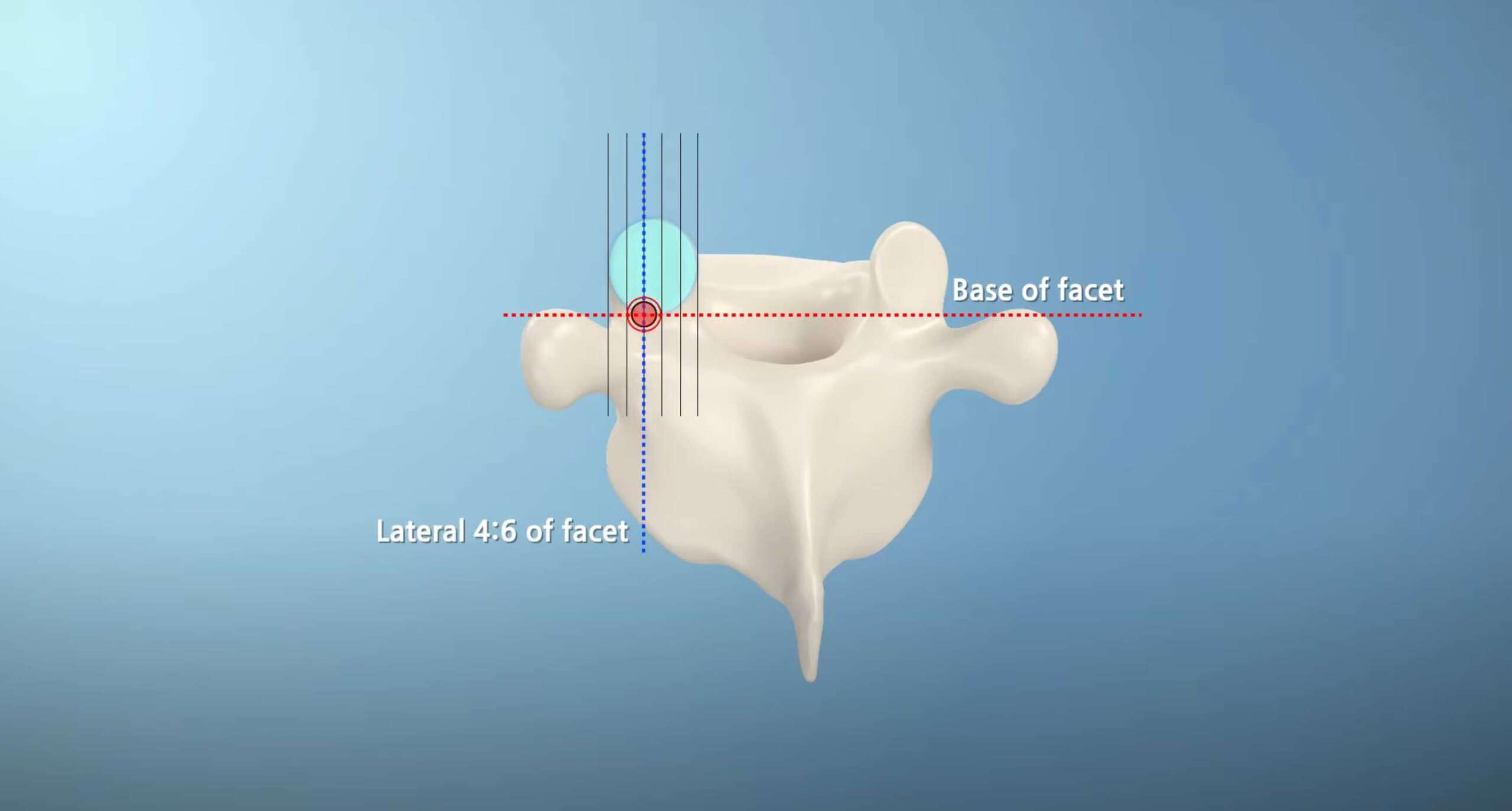
Why millimeters matter
The pedicle corridor is narrow — just 4–7mm in diameter. A single millimeter off course can mean the difference between a safe placement and serious complications.
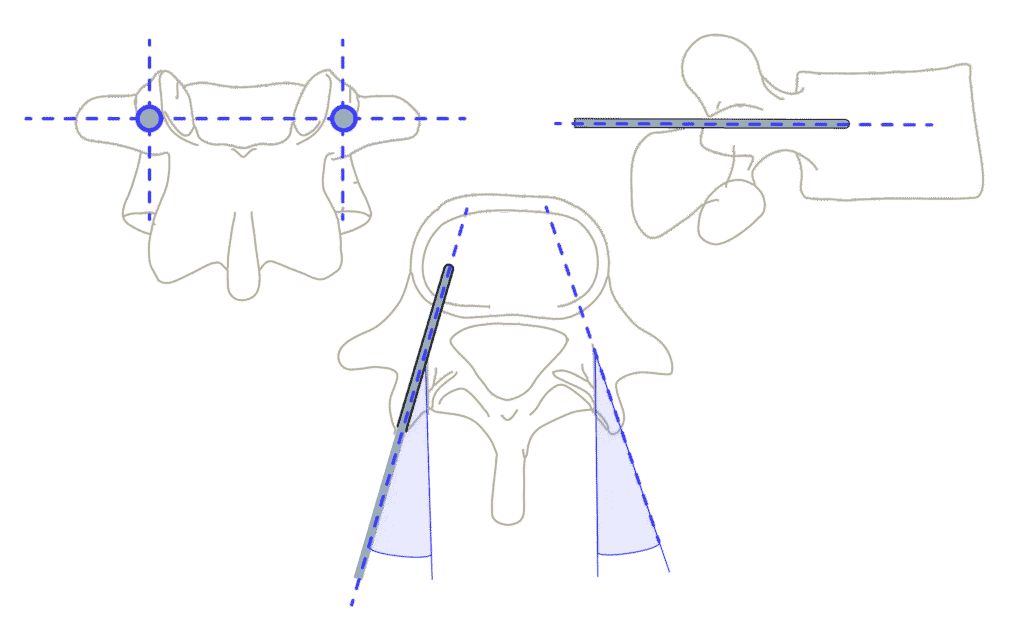
Critical anatomical considerations
Pedicle screws must avoid the spinal cord (medial), nerve roots (lateral), and major vessels (anterior)
Whatever your challenge — patient safety, surgeon safety, learning-curve or surgical efficiency — if it matters to you, we’ve built the solution.
Pedicle screw malalignment
“Do no harm”
Sokrates
Of course, these never happen…
- Spinal cord injuries and neurological damage
- Major vascular perforations
- Mechanically unstable constructs
- Extended hospital stays and patient suffering
Pedicle screw errors continue to cause avoidable complications and costly revisions – problems patients shouldn’t have to face.
Navigation and robotic systems are not immune; while 90-day revisions for pedicle malalignment for these systems is less than 1%, intraoperative revisions due to misplacement is up to 3%.
- Veeravagu (2014) - Meta-analysis of pedicle screw complications in spine surgery
- Staartjes World Neurosurgery (2018) - Long-term outcomes of pedicle screw misplacement
- Bindels GSJ (2024) - Economic impact of revision spine surgery
Freehand Revision Cost Calculator
Calculate the potential annual costs of revision surgeries from freehand pedicle screw placement in your facility.
intraoperative revisions
due to misplacement even with navigation/robotics
>$2B
per year in extra expense globally
4–6%
of freehand surgeries require a revision
Excessive radiation exposure
Flooding the OR with X-rays and CT scans for screw checks is a dangerous and somewhat dated habit — putting surgeons, staff, and patients at needless risk of radiation damage.
Surely, there’s a smarter way…
- Cumulative exposure drives cancer, cataracts, thyroid disease
- Chronic radiation causes fatigue, impairs focus and clinical judgement
- Pediatric patients face higher lifetime risk
- Lead aprons are heavy, exhausting
- Asari J. Orthop. Sci. (2022) - Radiation exposure risks in spine surgery
- Mastrangelo, Occ. Med. (2005) - Occupational cancer risk in surgical specialties
- Rampersaud et al. (2000) - Radiation exposure during spinal surgery
Spine surgeons have a
greater cancer risk
Surgeons often exceed lifetime dose limits (e.g. hands, thyroid, whole‑body) even when annual levels appear compliant
Navigation and robotics shift radiation from surgeon to patient.
Intraoperative CT delivers 3–10× higher doses than fluoroscopy — hundreds of chest X-rays in one case.
Staff are safer, but patients, especially the young, face unnecessary long-term cancer risk.
Workflow interruptions
Surgeons face relentless pressure to operate faster, turn cases around quicker, and maximize OR throughput — yet every unnecessary delay makes that impossible.
Technology can increase workflow challenges…
- Wasting OR minutes – extends OR time and costs
- Frequent C-arm repositioning interrupts surgical workflow
- CAS systems time-consuming setup wastes OR minutes
- One patient shift = full recalibration of CAS systems
- Veeravagu (2014) - Meta-analysis of pedicle screw complications in spine surgery
- Staartjes World Neurosurgery (2018) - Long-term outcomes of pedicle screw misplacement
- Bindels GSJ (2024) - Economic impact of revision spine surgery
OR Time Lost – Calculators
- Asari J. Orthop. Sci. (2022) - Radiation exposure risks in spine surgery
- Mastrangelo, Occ. Med. (2005) - Occupational cancer risk in surgical specialties
- Rampersaud et al. (2000) - Radiation exposure during spinal surgery
- Asari J. Orthop. Sci. (2022) - Radiation exposure risks in spine surgery
- Mastrangelo, Occ. Med. (2005) - Occupational cancer risk in surgical specialties
- Rampersaud et al. (2000) - Radiation exposure during spinal surgery
Wasted OR Time – Robot Setup
4–6
hours/month*
The equiavlent of 1-3 extra surgeries per month
* Drape, boot, register, plan, arm positioning (15-25mins) – 4 spine surgeries per week requring precision pedicle screw placement
Last 2 millimeters: The look-ahead challenge
Pedicle screw placement is a game of millimeters. Accuracy in the final 2 mm before cortical breach is what separates safe, stable fixation from nerve injury, revision surgery, or worse.
Why It’s a Problem
- Freehand techniques: Surgeons rely on feel and fluoroscopy. Neither provides reliable warning in the last millimeters.
- Navigation and Robots: These systems project planned trajectories from pre- or intra-operative imaging. But once the spine shifts, or a reference frame moves, the screen may not reflect reality. They do not sense bone quality in real time—so the last 2 mm remain blind.
- Dynamic Surgical Guidance (DSG) Technology: The DSG probe listens for changes in electrical conductivity, but only at the tip. That means feedback comes too late—when a breach may already be unavoidable. Signal interpretation can also be inconsistent, especially in bleeding bone or revisions.
Prohibitive capital investment barriers
Navigation and Robotic systems reduce complication rates to between 0.7% and 0.9%; however, they require sizeable upfront investment, and have high annual maintenance costs.
It’s not all roses…
- Prohibitive capital + recurring costs
- Hidden workflow tax
- Modest absolute risk reduction in many cases c.f. new smart instruments
- Surgeon autonomy & skill erosion
- Operational fragility & radiation trade-offs
- 2020 Millennium Research Group - Global spine device market analysis
- Biospace (2022) - Healthcare technology adoption barriers
- Grandview Research (2024) - Spine surgery market accessibility study